In a stark warning for global health, a new study estimates that antibiotic-resistant infections, often referred to as “superbugs,” could claim nearly 40 million lives by 2050 if decisive action is not taken. These alarming projections underscore the growing menace of antimicrobial resistance (AMR), which is emerging as one of the most significant threats to modern medicine.
The Growing Threat of Superbugs
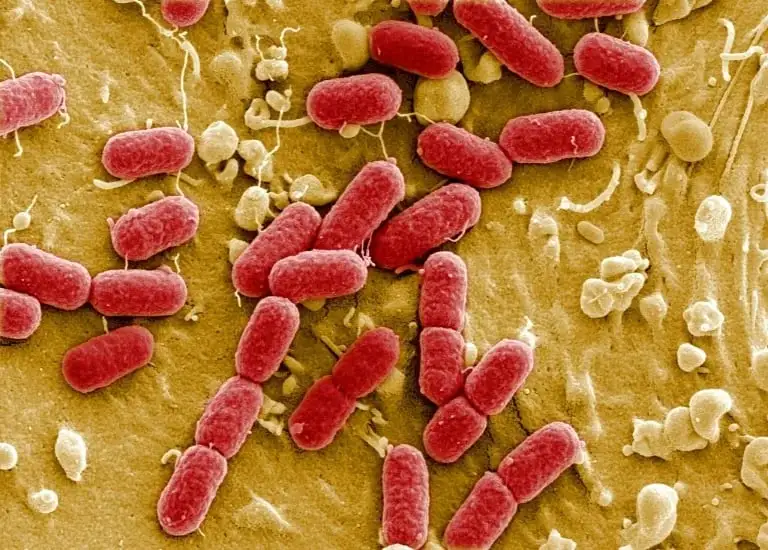
Superbugs are bacteria and fungi that have evolved to resist the effects of antibiotics and other medications. These pathogens thrive as a result of overuse and misuse of antibiotics, both in healthcare and agriculture. Once treatable infections such as pneumonia, tuberculosis, and urinary tract infections are becoming more difficult, and sometimes impossible, to treat.
The World Health Organization (WHO) has long identified AMR as a top global health threat, warning that it could push modern medicine back into a “pre-antibiotic era,” where routine surgeries, minor infections, and childbirth carry life-threatening risks. The study in question, which aggregates data from several health agencies and research institutions, takes these concerns further, estimating that the crisis could cause more deaths annually than cancer by mid-century.
Key Findings of the Study
The study, which involved a global consortium of scientists and health economists, analyzed the impact of AMR on healthcare systems, patient mortality, and economic stability. According to the findings:
- 40 Million Deaths by 2050: If current trends continue, antibiotic-resistant infections could kill 40 million people worldwide by 2050, particularly affecting regions with weaker healthcare infrastructure.
- Developing Nations at Highest Risk: Low-income countries, especially in sub-Saharan Africa and Southeast Asia, are expected to bear the brunt of this crisis. Limited access to healthcare, unregulated antibiotic use, and inadequate sanitation all contribute to the rapid spread of drug-resistant infections in these regions.
- Economic Consequences: The global economic impact of AMR could rival that of the 2008 financial crisis. If left unchecked, drug-resistant infections could cost the global economy up to $100 trillion over the next 30 years, with industries like agriculture, travel, and healthcare particularly vulnerable.
- Common Infections Becoming Lethal: Simple infections, once easily curable, are already becoming fatal in some cases. For example, sepsis and bloodstream infections caused by resistant bacteria are on the rise, especially among immunocompromised individuals.
Factors Driving the AMR Crisis
The rise of antibiotic resistance is linked to several key factors:
- Overprescription of Antibiotics: In both human medicine and agriculture, antibiotics are often overprescribed. For example, antibiotics are still frequently given for viral infections like colds and the flu, despite their ineffectiveness against viruses.
- Lack of New Antibiotics: The development of new antibiotics has significantly slowed down in recent decades. Pharmaceutical companies often shy away from investing in antibiotic research due to the high costs and low financial return compared to other medications.
- Inadequate Regulation: In many parts of the world, antibiotics are available over-the-counter without a prescription, leading to widespread misuse. The lack of standardized guidelines and enforcement contributes to improper antibiotic use and rising resistance levels.
- Globalization and Travel: Increased international travel and trade make it easier for resistant bacteria to spread across borders. Superbugs that emerge in one part of the world can quickly become a global problem.
Impact on Healthcare Systems
The consequences of the superbug crisis extend beyond individual health risks, posing a significant burden on healthcare systems worldwide. Hospitals and clinics are already grappling with rising costs and longer treatment times for patients with drug-resistant infections. When first-line antibiotics fail, healthcare providers are forced to resort to more expensive, less effective, or more toxic drugs, driving up costs and complications.
Surgeries, organ transplants, cancer treatments, and even routine medical procedures rely heavily on antibiotics to prevent infections. Without effective antibiotics, these procedures become much riskier. The threat of widespread infection also limits hospitals’ capacities, leading to overcrowded emergency rooms, longer wait times, and higher mortality rates.
In low-resource countries, where healthcare systems are already underfunded, the strain of dealing with drug-resistant infections can be catastrophic. Limited access to diagnostic tools, lack of proper hygiene practices, and overcrowded hospitals create an environment ripe for the spread of superbugs.
Antibiotics in Agriculture: A Major Contributor to Resistance
One of the most significant contributors to the AMR crisis is the use of antibiotics in agriculture. Globally, antibiotics are commonly used to promote growth and prevent disease in livestock and poultry, often as a preventive measure in otherwise healthy animals. This practice is particularly prevalent in industrial-scale farming.
This widespread use contributes to the development of resistant bacteria, which can be transmitted to humans through food, water, and environmental exposure. The resistant bacteria can also spread between animals and humans, exacerbating the AMR problem.
In response, several countries have introduced regulations to curb the use of antibiotics in animal farming, including bans on growth-promotion antibiotics. However, in many regions, enforcement remains weak, and antibiotic use in agriculture continues to be a significant driver of resistance.
The Role of Pharmaceuticals in the Superbug Crisis
While overprescription and agricultural misuse are major contributors to AMR, the pharmaceutical industry’s reluctance to invest in new antibiotics also plays a significant role. Developing new antibiotics is a costly and time-consuming process with limited financial incentives. Unlike drugs for chronic conditions, which patients take over long periods, antibiotics are typically prescribed for short durations, making them less profitable.
As a result, fewer pharmaceutical companies are investing in antibiotic research. The pipeline for new antibiotics is nearly dry, with only a handful of promising drugs currently in development. This shortage leaves doctors with limited options when dealing with resistant infections.
Governments and global health organizations are calling for new incentives to spur innovation, such as public-private partnerships, grants, and financial rewards for companies that develop effective new antibiotics.
Global Strategies to Combat Antimicrobial Resistance
Experts stress that combating AMR requires a multi-pronged approach, combining efforts from governments, healthcare providers, and pharmaceutical companies. The key areas of focus include:
- Stewardship Programs: Hospitals and healthcare systems must implement antimicrobial stewardship programs to ensure that antibiotics are used appropriately. These programs aim to reduce overprescription and encourage the use of alternatives when possible.
- Innovation in Drug Development: There is an urgent need to invest in research and development for new antibiotics, alternative therapies (such as phage therapy), and diagnostic tools that can help identify infections quickly and accurately.
- Public Awareness and Education: Public health campaigns are essential to raise awareness about the dangers of antibiotic misuse. Education efforts should target both patients and healthcare providers to reduce unnecessary antibiotic prescriptions.
- Global Cooperation: AMR is a global issue that requires international collaboration. Strengthening regulations on antibiotic use, sharing data on resistant infections, and funding research are all necessary components of a unified response.
Can We Reverse the Trend?
While the situation is dire, there are reasons for hope. Countries that have implemented strict antibiotic regulations and stewardship programs have seen success in reducing resistance rates. For example, in Sweden, antibiotic consumption in both humans and animals has been drastically reduced through stringent guidelines and public health campaigns.
Furthermore, there is growing momentum around alternative treatments. Phage therapy, which uses viruses to kill bacteria, is showing promise in treating drug-resistant infections. Advances in diagnostics and artificial intelligence are also helping healthcare providers identify infections more quickly, allowing for more targeted treatments.
What Lies Ahead?
The superbug crisis, if not addressed, could spell disaster for public health systems across the globe. While the COVID-19 pandemic has brought renewed focus to infectious diseases, experts caution that AMR is a slow-burning crisis with the potential for long-term devastation. Unlike the novel coronavirus, AMR’s growth is insidious, and without immediate intervention, the world could face a future where routine infections become deadly once more.
In response to these findings, global health organizations are calling for increased funding, stricter regulations, and a collective effort to curb antibiotic resistance before it spirals out of control. With lives on the line, the battle against superbugs must be fought with urgency and innovation.
Key Takeaways
The sobering predictions about superbugs serve as a wake-up call for humanity. As we inch closer to a possible post-antibiotic era, the need for urgent action has never been more critical. Without a coordinated, global effort to combat AMR, the death toll could be staggering, and the progress of modern medicine could be undone. Governments, the healthcare industry, and individuals alike must come together to prevent a looming global health catastrophe.